Validate
The Validate process verifies various columns to ensure the data is cleaned and in a standardized format.
Starting the Validate Process
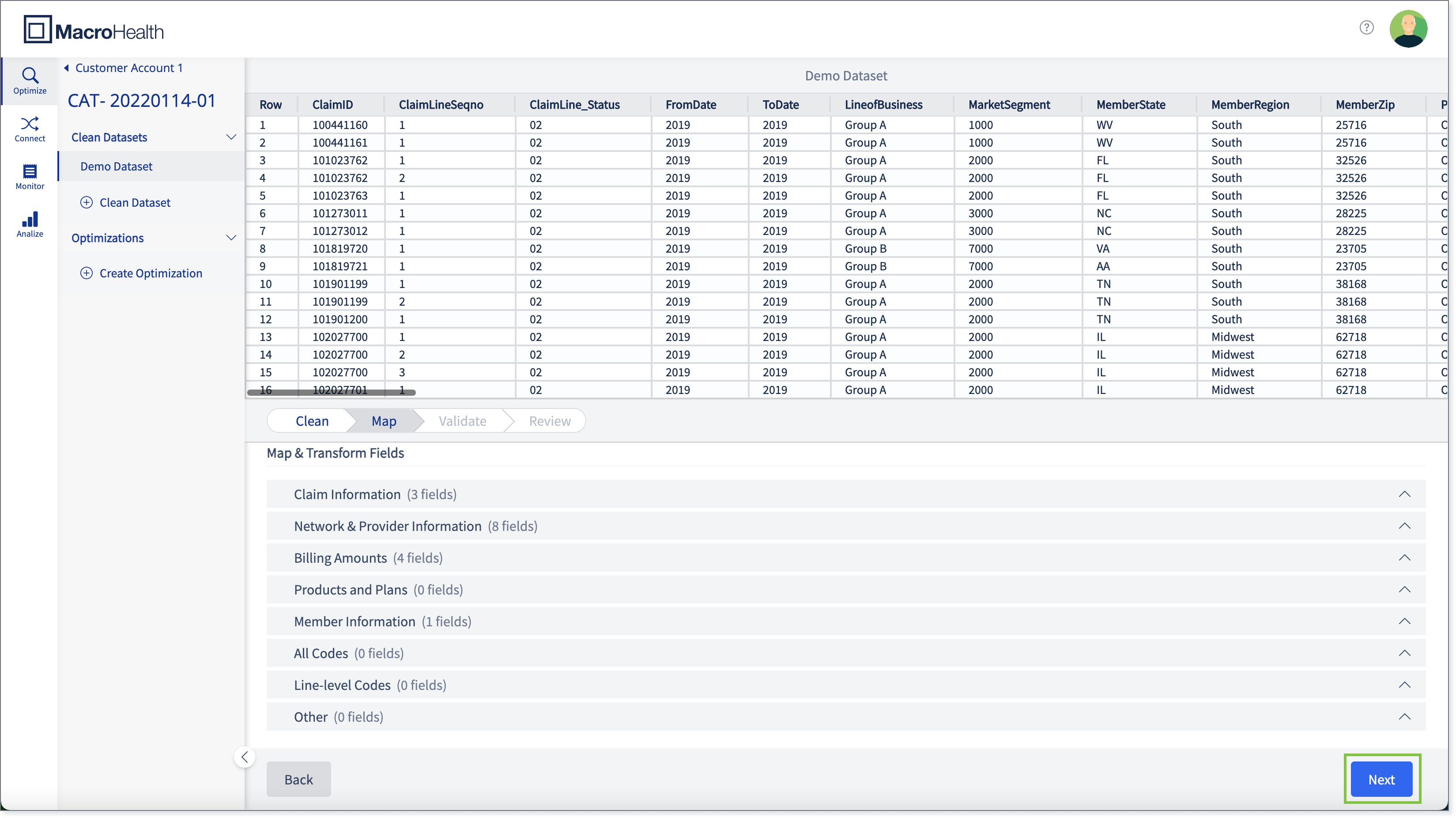
Once the Map process is completed, click Next.
Note
Once the "Next" button is clicked, it will be disabled and replaced with a spinner to inform you that the validation process is in progress.
The data file will go through the validating process.
Note
If you exit the browser, the validation process will continue to run in background. Once you return to the same dataset, if the validation is till in progress, you will remain on the Validation window, and if it is completed, you will land on Review.

The Validation Results will be displayed.

Validation Results
Checks on various columns to ensure the data is cleaned and in a standardized format.
Tip
For both Internal and External NOA, the required fields are validated and therefore, the number of claims/rows that are valid are displayed. And if a field(s) is missing, the Validation will display Fail, and the list of missing fields that are required in order to pass validation.
It may be necessary to request the missing information from the prospect.
Notice
For certain required values that have not been provided by the prospect, the NOA tool validates the information by deriving the value from other fields, such as the Provider County which derived form the Provider ZIP code or the Member County which is derived from the Member ZIP code.
Internal NOA
The process for estimating networks and vendors' repriced values for a given prospect claims file in-house.

External NOA
The process for reaching out to the Networks and OON vendors to obtain repriced a given prospect’s claim file.

Total Modified
Any values that were updated to be in the correct format or automatically derived from other values.

Total Exclusions
Invalid value that will result in the claim being excluded from the output.
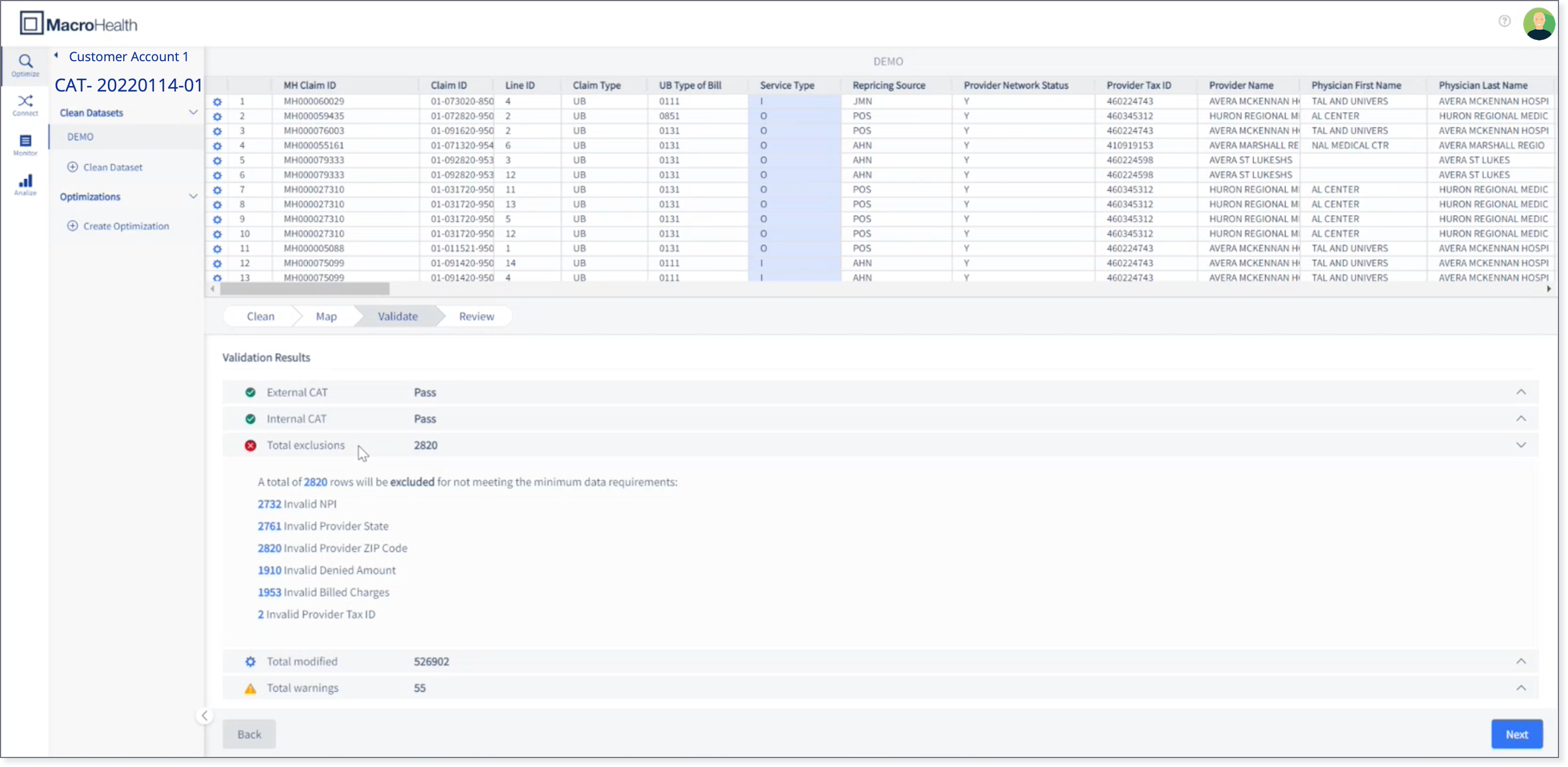
Total Warnings
Any values that are not required for repricing, but may not be in the correct format.

Interpreting the Preview Pane
Red: If a cell is invalid and causes the claim to be excluded from the final output. The whole row will be highlighted in red and the individual cell will be highlighted in a darker shade of red.

Yellow/Orange: If a cell was classified as a warning, the cell will be highlighted in yellow/orange.
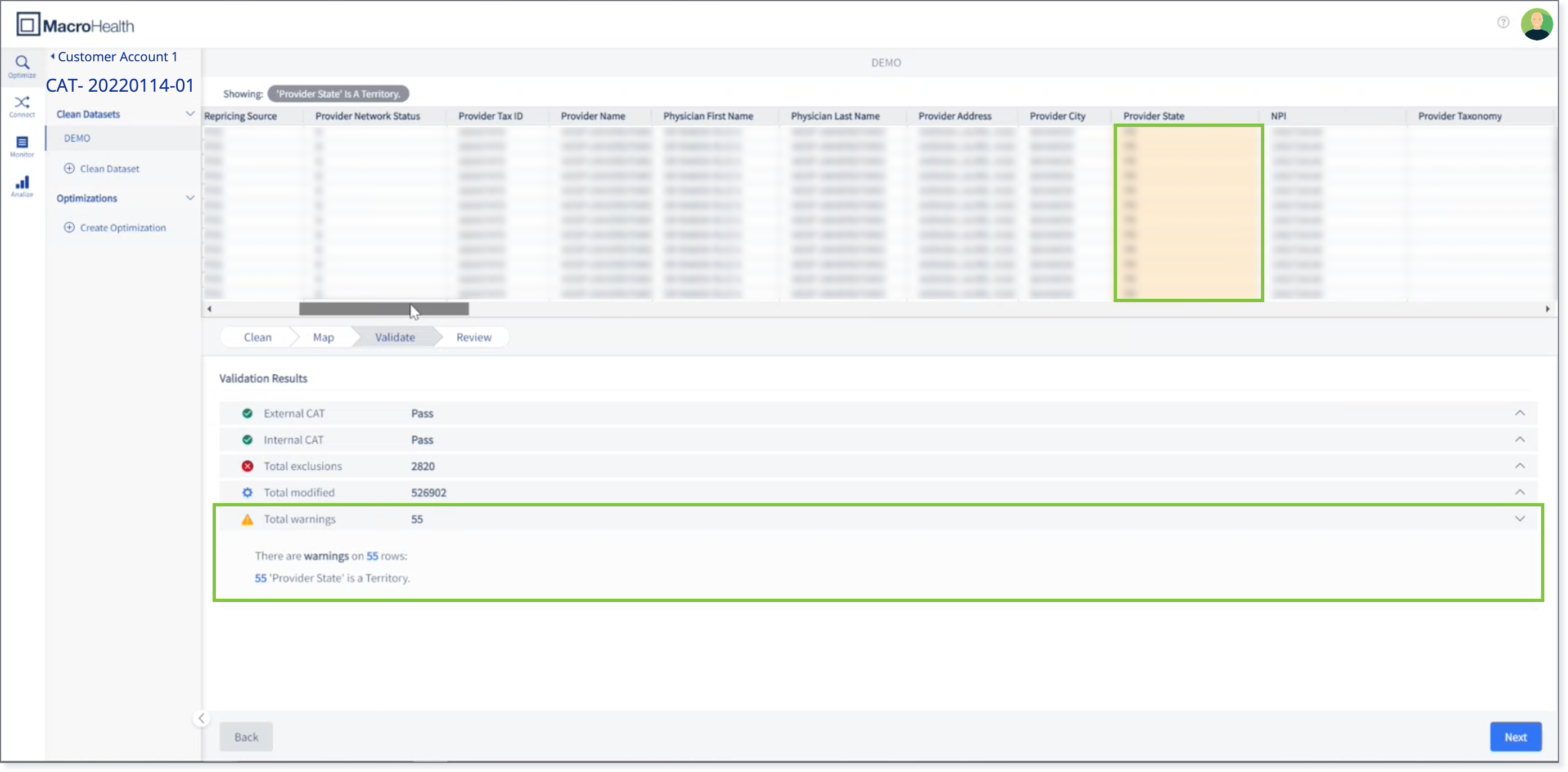
Blue: If a cell was modified (normalized to certain length or derived), the cell will be highlighted in blue.

Note
If a cell has one or more of the above, the individual cell highlighting is prioritized by the following order: Exclusion > Warning > Modified.
Filtering Down the Data File Preview
It is possible to filter down the data in the preview to only see the information that is relevant to what you are looking for.
Expand the Validation Result section required.

Click on the value corresponding to the filter that you want to view.

The filtered data can be viewed in the preview.
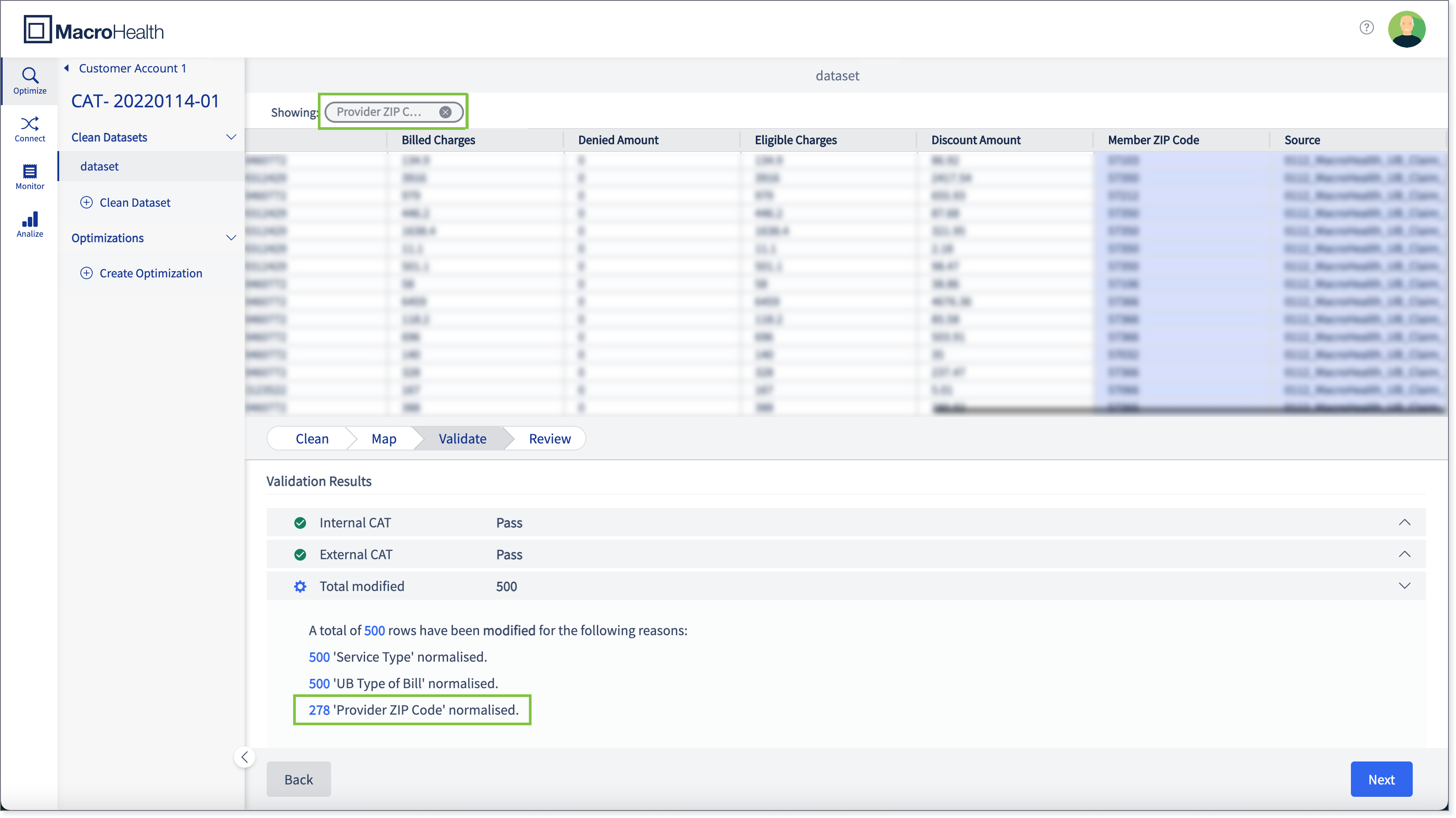
Tip
You can also remove the filtered data by clicking the X on the pill, which is the filter criteria highlighted in green in the above image. Removing it will reload the preview pane without any filters applied.
General Validation
The tool validates the dataset using pre-defined logic.
For each row, check the values of the following fields to determine if they are valid or invalid. An invalid value results in the claim/row to be excluded from the final dataset.
In the validation process, values are modified, normalized, and/or derived. The order of validation is as follows:
Note
The current validation process does not validate fields against other fields within the same claim. For example, it does not verify if 90210 (Provider Zip Code) is in CA (Provider State), but it validates that each value (90210 and CA) is individually valid.
Note
When prospects provide files with NULL as values, the NULL string value needs to be converted to an empty value. This applies for types of prospects: prospect, Network, and OON.
Once the tool validates each value, the tool validates the aggregation of a claim. By combining rows with the same Claim ID, it checks the following fields:
Values | Fields |
|---|---|
Negative Amounts | Billed Charges Denied Amount Eligible Charges |
Uniqueness | Claim Type Service Type Provider Tax ID Provider State Provider ZIP Code NPI |
MacroHealth Claim ID
Within a customer account, the tool generates a MH Claim ID, starting with MH000000001, for each unique Claim ID that is mapped.
This is important within the same NOA request workspace because it is used to reference the original claim from a Network or OON vendor repriced file.
The counter will restart at the one billionth claim for that customer account.
UB Type of Bill
If less than four characters, pad left with 0s
The value is invalid if it does not match any of the following:
First digit is a 0
Second and third digit is a number between 1 and 9
Fourth digit can be a number between 0 and 9 or a letter between A and Q
Revenue Code
Must be a three-to-four-digit number (each digit is between 0 and 9)
If only three digits, pad left with 0s to make it a four-digit number
Otherwise, the value is invalid
Service Type
If there is a value, uppercase and trim to the first letter
Else, if there is no value or the trimmed letter is not I, O or P
Check if Type of Bill has no value
Check if Line Level and Revenue code is mapped
If Revenue code is empty, assign Professional
If Revenue Code is greater than or equal to 0100 and less than or equal to 0219, assign Inpatient
Otherwise, assign Outpatient
Else assign Professional
Otherwise Type of Bill has a value
If any of the following, where X can be any value
011x
018x
021x
028x
032x
041x
065x
066x
086x
Assign Inpatient
Else, assign Outpatient
Then trim to the first letter, which results in I, O, or P
Claim Type
Remove any non-letters from the value (i.e.: 123ABC becomes ABC) and capitalize
If it is not empty, keep value
Else, if it is empty, check Service Type
If Service Type = Professional, assign HCFA
Else, assign UB
Provider Tax ID
Remove any dashes and underscores
Value is invalid if it:
Is empty
Contains a letter
Consists of one repeating digit (111111111)
Is less than 7 digits
Is greater than 9 digits
Pads value with leading 0s to make it 9 digits
Provider State
Convert string to uppercase
If it’s not abbreviated, convert to abbreviation based on the list state names
State is invalid if:
No value
Armed Forces
Does not match the list of abbreviated states
State has a warning if:
Territory
State List
State | Abbreviation | Notes |
|---|---|---|
Alabama | AL | |
Alaska | AK | |
American Samoa | AS | Territory |
Arizona | AZ | |
Arkansas | AR | |
California | CA | |
Colorado | CO | |
Connecticut | CT | |
Delaware | DE | |
District of Columbia | DC | |
Federated States of Micronesia | FM | Territory |
Florida | FL | |
Georgia | GA | |
Guam | GU | Territory |
Hawaii | HI | |
Idaho | ID | |
Illinois | IL | |
Indiana | IN | |
Iowa | IA | |
Kansas | KS | |
Kentucky | KY | |
Louisiana | LA | |
Maine | ME | |
Marshall Islands | MH | Territory |
Maryland | MD | |
Massachusetts | MA | |
Michigan | MI | |
Minnesota | MN | |
Mississippi | MS | |
Missouri | MO | |
Montana | MT | |
Nebraska | NE | |
Nevada | NV | |
New Hampshire | NH | |
New Jersey | NJ | |
New Mexico | NM | |
New York | NY | |
North Carolina | NC | |
North Dakota | ND | |
Northern Mariana Islands | MP | Territory |
Ohio | OH | |
Oklahoma | OK | |
Oregon | OR | |
Palau | PW | Territory |
Pennsylvania | PA | |
Puerto Rico | PR | Territory |
Rhode Island | RI | |
South Carolina | SC | |
South Dakota | SD | |
Tennessee | TN | |
Texas | TX | |
Utah | UT | |
Vermont | VT | |
Virgin Islands | VI | Territory |
Virginia | VA | |
Washington | WA | |
West Virginia | WV | |
Wisconsin | WI | |
Wyoming | WY | |
Armed Forces America | AA | Armed Forces Region |
Armed Forces Europe | AE | Armed Forces Region |
Armed Forces Pacific | AP | Armed Forces Region |
Provider Zip Code
Sets as invalid if the value has greater than 9 numeric digits
If only 5 digits, sets value as the same 5 digits
Otherwise:
If less than 5 digits, pads left with 0s
If greater than 5 digits, left pad with 0s to 9 digits then take the first 5 digits
Compares value to the zip code database
Invalid if no value or there is no match in the zip code database
Zip Code Database Details
Source: https://www.zip-codes.com
Product: Zip Code Database – Deluxe
Version: March 1, 2021
NPI
Remove any underscores or dashes
Value is invalid if:
Is empty
Contains a letter
Consists of one repeating digit (111111111)
Is not 10 digits
First digit is not 1
Pads value with leading 0s to make it 10 digits
Provider Network Status
Checks each value (case in-sensitive)
Value is set to “Y” if it contains any of the following:
"y"
"yes"
"in network"
"in-network"
"innetwork"
"national"
Value is set to “N” if it contains any of the following:
"n"
"no"
"out of network"
"out-of-network"
"outofnetwork"
Otherwise, value is invalid
Negative Amounts
Once each value has been validated, the claims are then aggregated by Claim ID. For each claim, the sum for each field is calculated.
If the sum is negative, the whole claim is considered invalid.
Uniqueness
Another validation when aggregating by Claim ID is verifying that it’s the same value among the lines. If they are not, the tool produces a warning and picks the first value when producing a claim level output.